While it is well accepted that medical-grade masks, such as the N-95 and N-99 masks, are effective in providing a barrier to COVID-19 droplet and aerosolization dispersal, many in the general public are relying on cloth-based coverings as a strategy to minimize the risk of cross-infection via respiratory droplets.

Respiratory droplets via coughing, sneezing, or even talking and breathing may contain COVID-19. Droplets can vary in size and their transport characteristics are contingent on this size. The smallest droplets can remain suspended indefinitely depending on the surrounding ventilation airflow. New studies have now evaluated the ability of cloth masks as a form of personal protective equipment.
As a general principle, the World Health Organization recommends that a mask’s shape should allow fitting over the nose, cheeks, and chin of the wearer.

This permits an efficient barrier to respiratory droplets. Further, cloth masks must have at least three layers. The inner layer absorbs any materials from breathing, coughing or sneezing, a middle layer that provides further filtration, and an outer layer made from a nonabsorbent material like polyester to protect against external contamination.
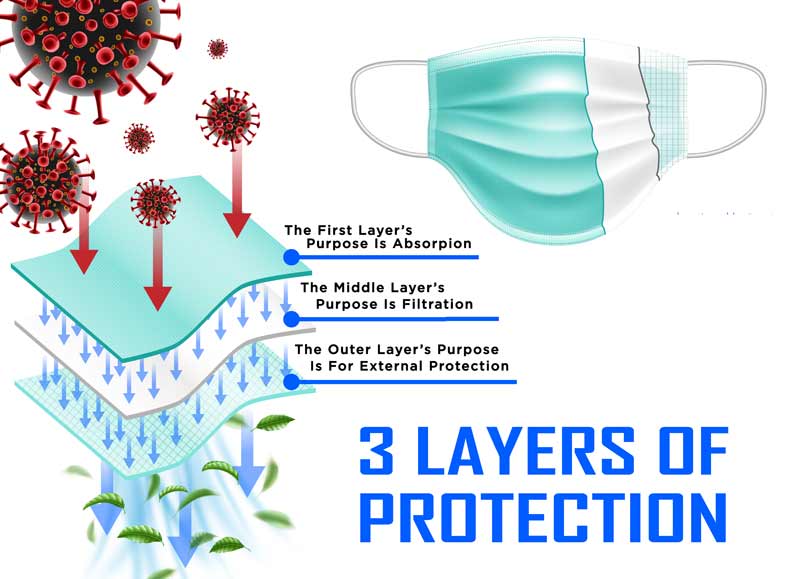
Other factors important in cloth mask effectiveness include thread count for cotton materials, type of fabric in each layer, and degree of water resistance for the innermost layer.
These recommendations are supported by the science. In one study that looked at cloth masks, a video was employed to observe emulated respiratory jets to evaluate the stopping capacity of various masks.

This study found that loosely folded face masks and bandana-style coverings possessed the poorest performance in stopping small aerosolized respiratory droplets. The best designs were those that were well-fitted with multiple layers of cloth fabric designed within the mask. Only small gaps along the edges of these masks allowed material to leak through. Interestingly, uncovered emulated coughs traveled greater than the recommended physical distancing of 6 feet.
Clinical experience also supports the effectiveness of cloth masks. A study published in the Lancet confirmed that masks reduced the incidence of COVID-19 transmission. Another study published in Health Affairs concluded that the use of face masks decreases the spread of COVID-19. Finally, with respect to COVID-19 death rates, the use of masks was associated with a lower rate of mortality.
The compelling part about the proper use of cloth face masks during this time comes from a study that evaluated the effects of universal or near-universal (80%) wear of face masks. The study implemented a theoretical simulation model and found that at least 80% masking in a population significantly lowers rates of COVID-19 transmission. At a rate of 50% compliance, however, suppression of daily COVID-19 case growth is not successful. This suggests that if the goal is to move away from the “full-body” lockdown with its substantial economic and social effects, then it might be advisable to accept a “mouth and nose” lockdown through the proper use of cloth masks.

Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.