In this time of social isolation brought on by the COVID-19 pandemic, many are attempting to pass the time with an exercise routine that respects the “6-foot-rule.” Also, where appropriate, an exercise routine that incorporates the outdoors with fresh air and the ability to explore nature seems more palatable. Even where going outdoors is not achievable, there are countless homes where an old treadmill or exercycle has been collecting dust, looking for a reason to be used.
The time is now when we should see a revival in running and cycling activities. Accordingly, this review addresses a common injury in these pursuits — iliotibial band syndrome (ITB).
Iliotibial band syndrome is a common overuse injury. Pain is experienced at the outside, or lateral part of the knee.

The location of the pain appears to stem from the movement of the iliotibial band over a bony prominence of the knee called the lateral femoral condyle.
See Figure 2 which represents a front bony skeletal view of the pelvis and thighs
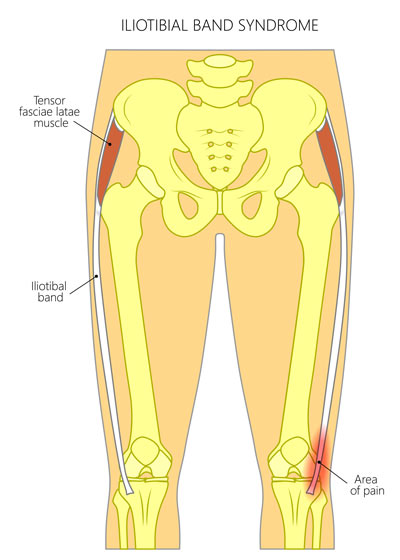
The iliotibial band itself extends from the side of the hip to the side of the knee. At the hip, it is associated with a group of muscles called the hip abductors. The hip abductors are responsible for moving the leg/hip away from the body and to the side.
See Figure 3 (bottom)
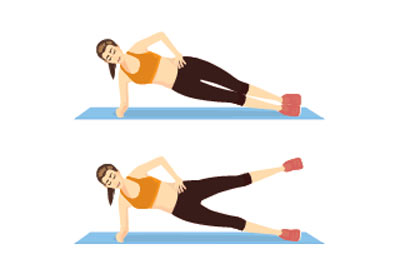
Hip abductor weakness is associated with ITB syndrome. Moreover, at the knee, iliotibial band thickening and inflammation has been observed.
Biomechanically in runners, it has also been found that the leg affected with ITB syndrome displays a motion with more hip adduction (or having the leg/hip move toward the body), and more knee internal rotation (or motion that causes the shin and foot to turn inward).

Prevention and treatment, therefore, rely on interventions that include strengthening of the hip abductors, stretching of the iliotibial band, neuromuscular re-education and anti-inflammation measures directed to the area of pain.
Consult your health care provider to determine if you are experiencing symptoms related to ITB syndrome and what treatment alternatives are available.
Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.