Concussions represent an injury to the brain caused by trauma. Another term for a concussion is a traumatic brain injury. The trauma can come from a direct blow to the head or sudden acceleration and deceleration of the brain inside the skull. The latter is also called a coup-contrecoup injury. Coup refers to the site of direct impact with an object, and contrecoup refers to the area on the opposite side of the direct impact.
An estimated 2.8 million individuals sustain a concussion or traumatic brain injury each year. Of those, 282,000 are hospitalized and 50,000 will die.
Symptoms of a concussion relate to the area of the brain where the impact occurred. As a result, a variety of symptoms may be reported such as headaches, nausea or vomiting, dizziness, light sensitivity, feeling “foggy,” and difficulty concentrating. Mood, behavior, and personality changes have also been noted.

The Centers for Disease Control have published danger signs and symptoms of a concussion that require emergent evaluation. These include one pupil being larger than the other;

drowsiness; a worsening headache that won’t go away; slurred speech, weakness, or numbness; repeated vomiting or seizures; and loss of consciousness, even if only for a brief period.
It is important to identify concussions because any subsequent traumatic brain injury may have more lasting effects if the initial effects of a first concussion are not allowed to resolve. This is more important in children because an immature brain does not recover as quickly as a mature brain.

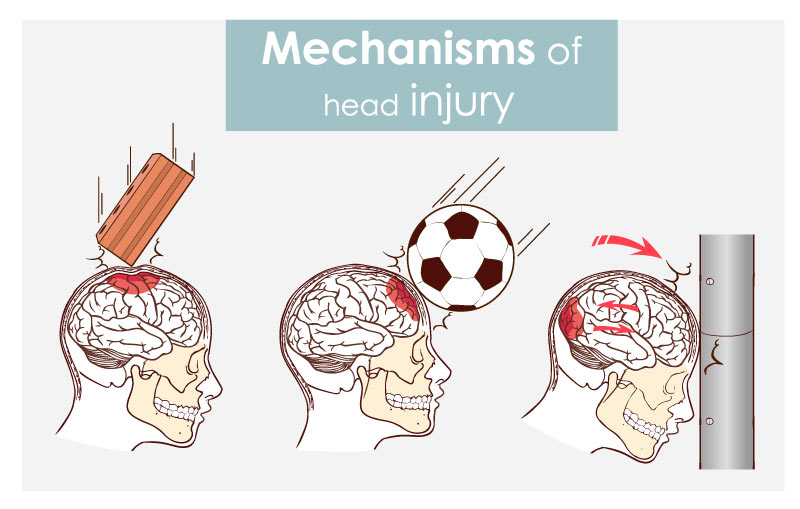
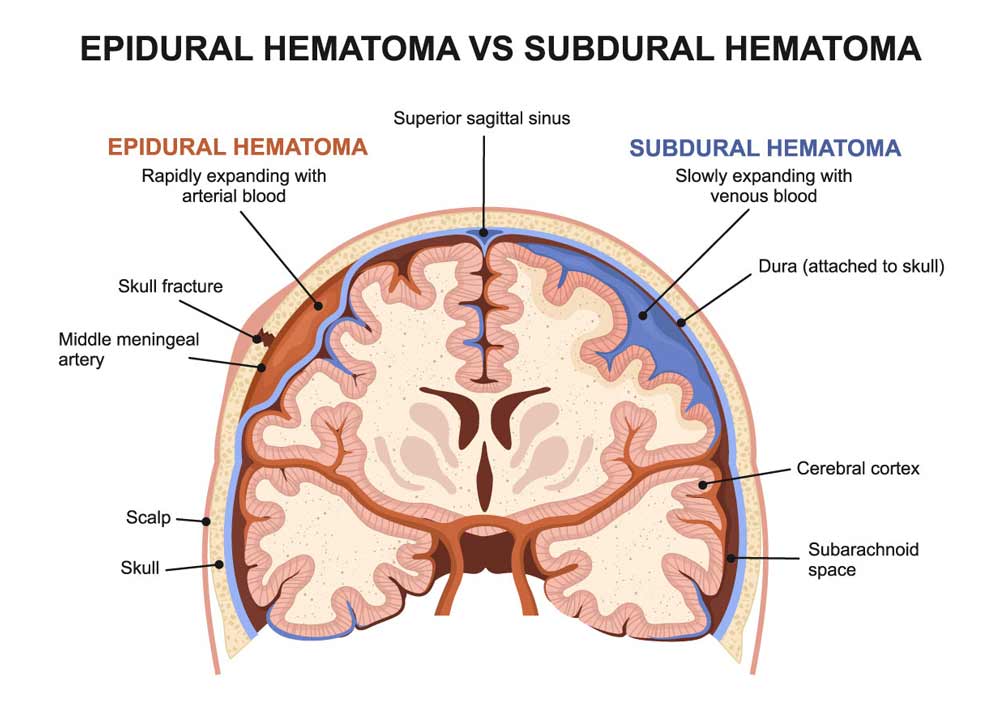
In addition to a doctor’s evaluation, imaging may help evaluate a concussion. Imaging can include CT scans and MRI, which can identify whether bleeding has occurred in the brain region, also called a subdural or epidural hematoma.
An even more tragic effect of an undiagnosed concussion is what has been called a second impact syndrome. In these cases, a second blow/concussion causes catastrophic brain swelling and subsequent death.
Because concussions can occur in organized activities, such as sporting events,

and because of individual variabilities in baseline brain function, pre-season or pre-activity testing is recommended to assess an individual’s balance and brain function prior to a suspected concussion and to later establish a concussion’s effects. It can also help aid in deciding when an individual can return to full activity.
Baseline testing may also include a computerized neuropsychological test.
One commonly used testing assessment tool is ImPACT. ImPACT refers to Immediate Post-concussion Assessment and Cognitive Test. This test is the only FDA-approved tool for concussion assessment. Testing areas include attention, speed of processing information, verbal memory, visual memory, visual motor speed, and multi-tasking ability. ImPACT is most specifically useful for measuring progress in concussion recovery.
On the horizon for helping to diagnose concussions include laboratory testing. One recent clinical study confirmed that the analysis of saliva may facilitate the diagnosis of a concussion by a medical provider.

The salivary analysis involves evaluating the presence of certain microRNA molecules. More research is necessary, but the use of laboratory testing as a tool could be a substantial step in diagnosing and preventing future injury.
Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.