Long-term care facilities, or nursing homes, are responsible for delivering safe care to their elderly residents. Typically, residents have neither the physical ability nor mental capacity to live independently. Residents rely on the nursing homes themselves to prevent undue exposure to danger, that includes infectious disease. With the advent of COVID-19 and its devastating effects, particularly on the elderly, a vigorous standard of protection must be maintained in long-term care facilities to avoid preventable tragedies.

Recently, it has been discovered that one Massachusetts Veteran’s Home (“Home”) did not comply with their obligations. As a result, 76 veteran nursing home residents unnecessarily died, contributing to the distressingly expanding death toll from COVID-19. Moreover, a backlash from employees of the Home has resulted in a Federal Class Action lawsuit against the former leadership of the Home. Specifically, the Home did not follow well-published public health recommendations, and its leadership made “substantial errors” in its decision-making capacity. An independent investigation by the Governor of Massachusetts described actions of the Home’s leadership as “utterly baffling.”
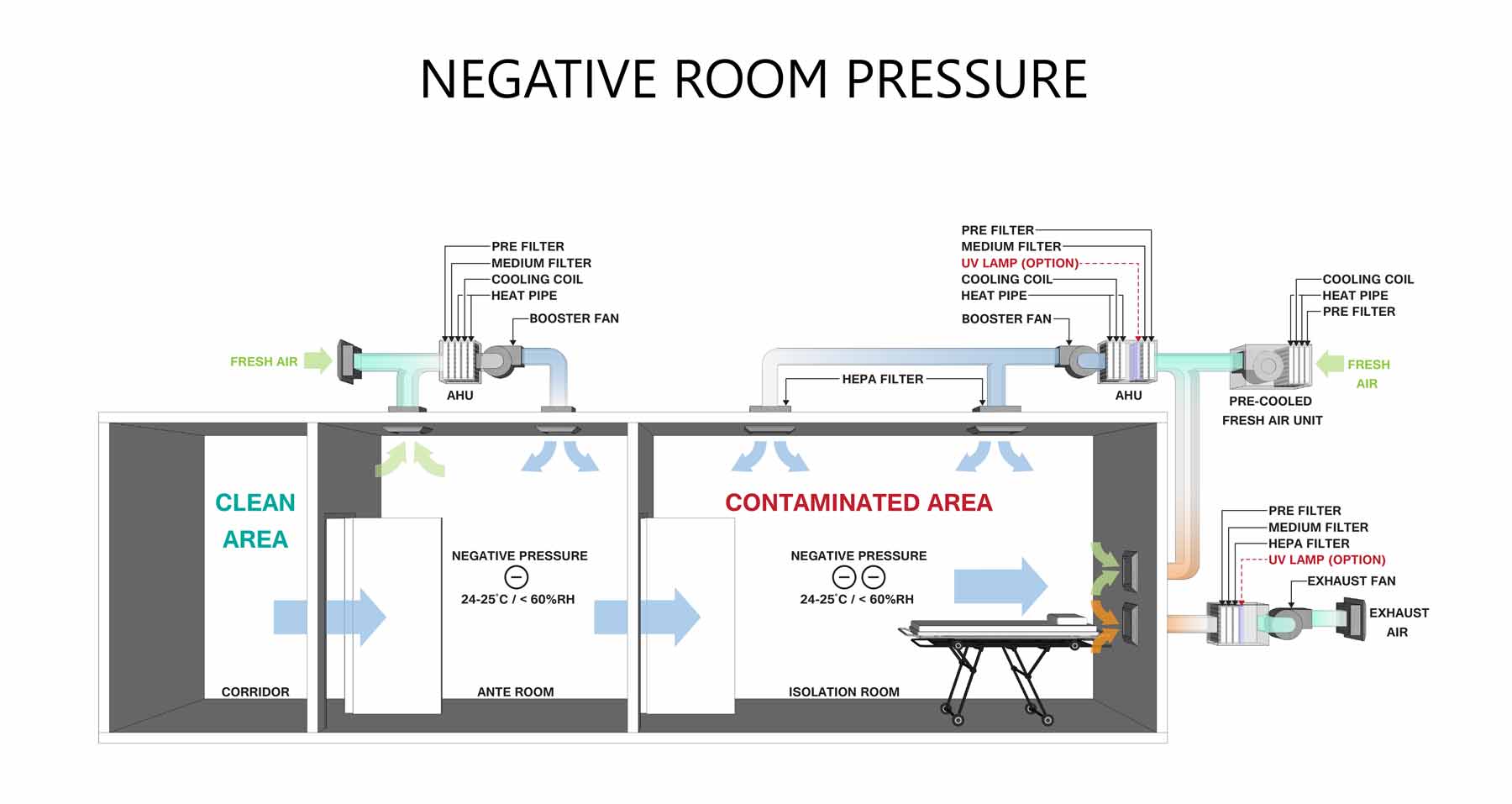
For example, a basic principle of infection control is to isolate those with disease from those without disease.

But the Home’s leadership team instead chose to move all its veterans from its two locked dementia units, into one unit alone. Notably, of the residents who were moved into the single space, some were veterans who tested COVID-19 positive, some were suspected of having COVID-19, and some had no COVID-19 symptoms whatsoever. Witness accounts described the scenes as veterans “crammed in on top of each other.” The Chief Nursing Officer of the facility, in what appeared to be an effort to conceal their actions, instructed social workers to contact resident’s family members to persuade them to change their advanced directives so no transfer to a hospital could occur.
Isolation of COVID-19 cases, whether suspected or confirmed, was required under the COVID-19 mandates published during that time by the Centers for Disease Control and Prevention (CDC).

and the Massachusetts Department of Public Health.
This Home did, in fact, have isolation rooms, but they were not utilized.
Much of the responsibility for the “baffling” decisions has been attributed to the Superintendent of the facility. The law in the Commonwealth requires that those managing a nursing home possess credentials as a licensed nursing home administrator.

In this case, however, the Massachusetts Department of Public Health waived this requirement because of the Home’s status as a state-run facility. So ultimately, this falls back on those overseeing the Superintendent.
As of September 12, 2021, there has been an estimated 652,894 deaths related to COVID-19. Although not all cases can be attributable to poor planning or careless response in long-term care facilities, in those cases where standards are in place to prevent such tragedies, careful scrutiny and investigation for preventive strategies are warranted.
Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.