Fever, dry cough and shortness of breath are the well-publicized symptoms related to COVID-19 infection. A more detailed look, however, may help us understand the spectrum of symptoms one might display after an infection.
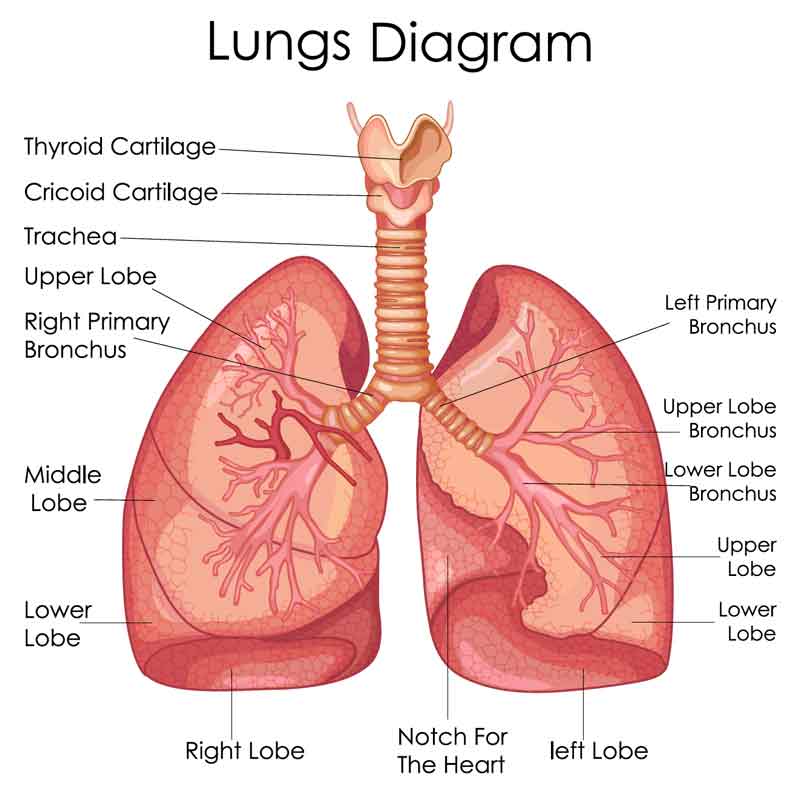
As a respiratory virus, COVID-19 symptoms develop as a result of a viral load to the respiratory system. The respiratory system allows us to breath oxygen and exhale carbon dioxide. It consists of an expanding tree of tube-like structures that conduct the transport of air and culminates in a gas-exchange unit.
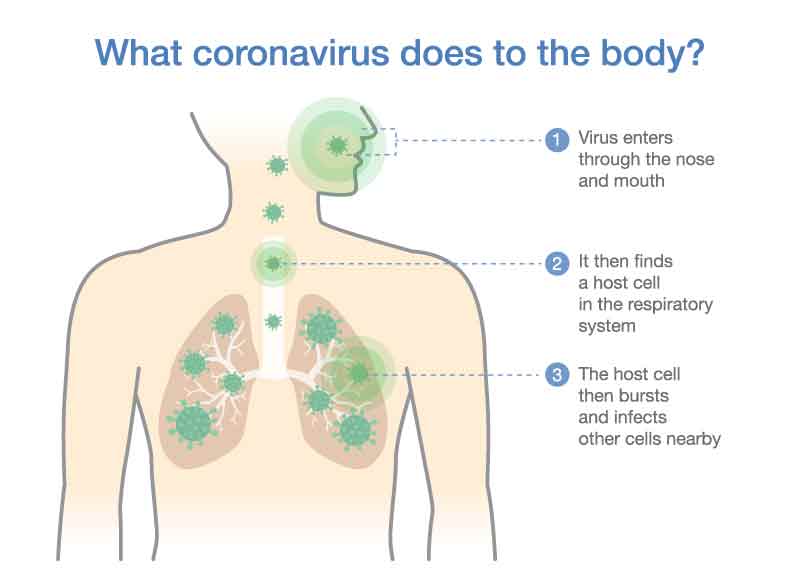
The virus itself injures by attacking the cells lining the tube-like structures and entering the cell.
Once inside the cell, it multiplies until the cell bursts. The virus can then infect other cells nearby.
The severity of an infection is related to the body’s ability to contain the virus’ spread—i.e how vigorous a body’s immune system can respond. Professor John Wilson, respiratory physician, categorizes those infected by COVID-19 into four broad categories based on severity:
1. individuals with sub-clinical infection—these individuals have the virus but do not exhibit symptoms.
2. individuals with minor symptoms—these individuals have an infection limited to the upper respiratory tract. Therefore symptoms include fever and cough, and perhaps a headache.
3. individuals with flu-like symptoms that usually keeps them out of work. This is by far the most common category.
4. individuals who develop a severe illness that features pneumonia. Pneumonia develops when the virus reaches the end of the respiratory tree where oxygen and carbon-dioxide are exchanged. Breathing is critically compromised.
The challenge of identifying COVID-19 in the elderly, however, is that symptoms in this population may be different from what is expected, or “atypical.”
The aging process and/or associated chronic illnesses may impair how this group responds to the infection. For example, a weakened immune response may disrupt a body’s ability to regulate temperature and mount a fever. Thus a fever may not manifest.
One geriatric physician in Switzerland has systematically catalogued atypical symptoms in the elderly that includes changes like delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain and the loss of smell and taste.
The point being that a high index of suspicion is necessary to identify and facilitate treatment in this population where COVID-19 effects are more severe.
Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.